The Struggle
It's Real
Sometimes hot flashes aren’t the main thing. Sometimes it’s more insidious. Outsized anxiety. Insomnia. Unshakable sadness. Disconnection from playfulness with a partner or a short temper with children. The feeling that she’s lost the core of who she was.
Maybe a prescription for an antidepressant is offered. Maybe some habit-forming sleeping pills or a benzodiazepine. Her concerns about perimenopause are dismissed because she’s still having periods. Her hormone levels are normal. It’s not her doctor’s fault that he wasn’t trained to recognize the signs.
This is the story of many of my patients. Some of them have spent months or years trying to figure out why their health seems to be falling apart.
The following is an interview with a friend. Her story isn’t mine to tell but you can read it here. Ally Iseman has graciously invited me to her monthly Open Dialogue LIVE session here on Substack Sunday, December 28 from 10:00 AM - 11:00 AM PST. We’ll discuss the emotional, cognitive and libido aspects of peri/menopause as well as the indications for and off-label use of testosterone in women.
Ally: What is perimenopause… in plain English?
Dr. Hull: Menopause is a retrospective diagnosis. It’s the day of a person’s life when it’s been exactly 1 year since their last menstrual period. But for a lot of patients this can be obscure. Patients who’ve had a hysterectomy, uterine ablation, Nexplanon or IUD may not experience periods at all. Patients who’ve experienced surgical menopause- hysterectomy with or without ovarian preservation- can experience some or all of the physiological consequences of menopause from the time of their surgery. Including significant deterioration of their bone density. Those patients absolutely need a conversation about starting hormone therapy post-operatively.
For women without a history of surgical menopause, I think of perimenopause as the years-long timeframe leading up to the last menstrual period when hormone production goes haywire. This graph is a nice visual. You can see that the hormone levels can be all over the place. This is why we don’t rely on blood testing to diagnose and treat perimenopause. Treatment is based on symptom management and the individual goals of the patient.
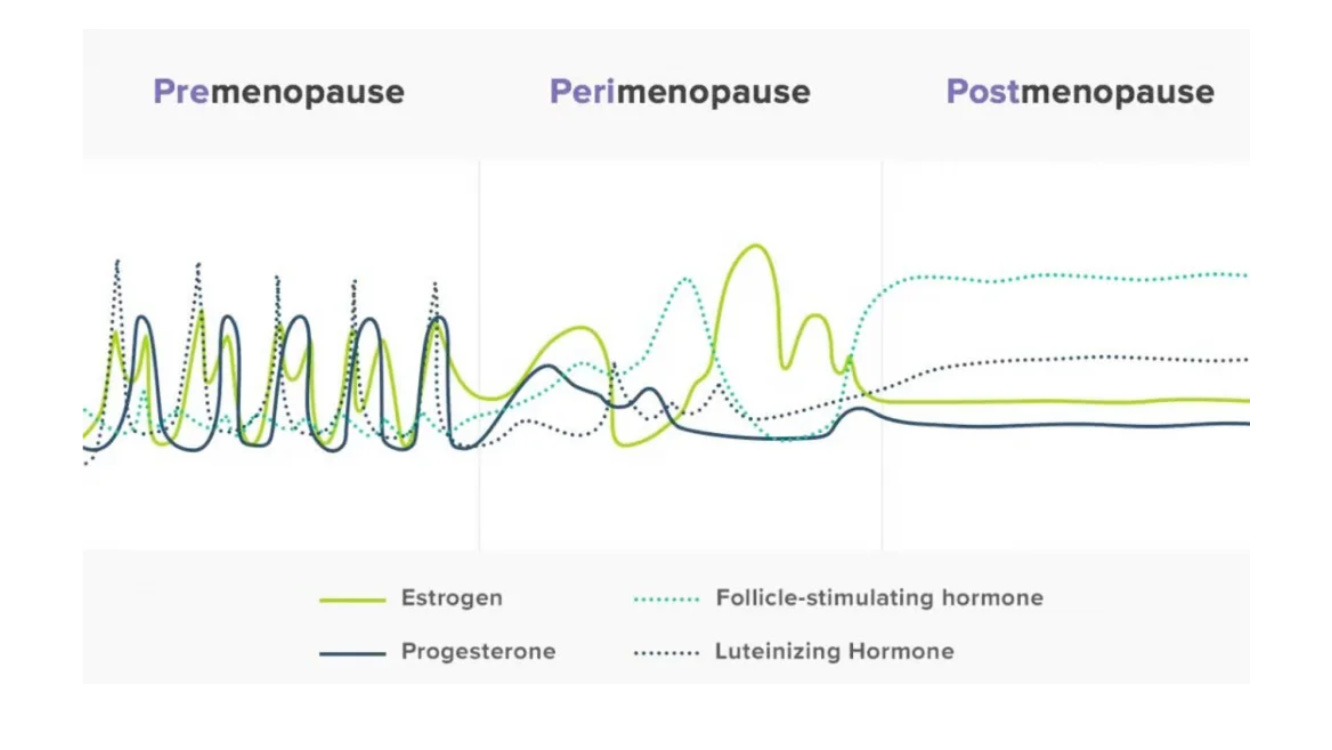
What used to be predictable cyclic hormone shifts become large swings in hormone levels. Patients can experience: heavy bleeding, early or late periods, decreased libido, depression/mood swings, poor sleep, weight gain, decreased bone mineral density, hair loss, increasing cholesterol, body aches/joint pain, vaginal dryness and brain fog in addition to hot flushes and night sweats. The constellation of symptoms, especially if she doesn’t experience hot flashes, is often diagnosed as depression or dismissed as trivial complaints that women should just deal with. But it really affects people’s quality of life in very tangible ways. Especially when it comes to professional confidence and interpersonal relationships. Women deserve to be heard and treated.
***It’s important to note that MHT is NOT contraception!***
Women in perimenopause who don’t have an IUD or some other form of long acting contraception are often offered oral contraceptives/birth control pills for this reason. OCPs can treat the symptoms of perimenopause while providing contraception. This is especially important to keep in mind in jurisdictions where women’s access to reproductive freedom is being restricted.
Guys should consider getting a vasectomy if they don’t desire additional children. I’ve had patients whose partners did so to facilitate their female partner’s treatment with MHT. I love hearing the words “my husband/partner is incredibly supportive.”
Ally: What’s the current state of menopause hormone therapy (MHT; formerly known as HRT)?
Dr. Hull: On November 12th, 2025, the United States Food and Drug Administration announced that it will remove the Black Box Warning labels from MHT products manufactured in the US. The Canadian Menopause Society supports this decision and has stated publicly that it, “will continue to engage with Health Canada and other Canadian interested parties to ensure labelling and guidance reflect up-to-date evidence and support informed choice for women across the country.”
As with any major scientific/medical policy announcement, there’s a lot of bickering and concern about both the political intentions and optics of this announcement. But I think the general consensus is that this policy decision will open the door to more open conversations about the individual risks/benefits of MHT for patients. And it will demand large-scale physician training/re-training efforts Which I think is a very good thing. I hope that there will also be robust institutional investment in woman’s health research going forward.
Here in BC, the University of British Columbia now has a curriculum for medical students. The Department of Continuing Professional Development is offering a course in February 2026 for practicing physicians.
In March of 2026, Canadian PharmaCare will begin offsetting the cost of MHT prescription medications. I’m proud that I live in a place that’s taking a leading role in this vital women’s health issue.
What can patients do?
Seek out trustworthy clinicians (ie: Menopause Society Certified Practitioners- MSCP). If your GP or family doctor doesn’t know much about this stuff, please understand that it’s not their fault. Menopause medicine wasn’t included in medical training for decades. Seek out someone who has undergone specific training in this area.
Expect a conversation about your individual risks and benefits. You may need some workup and monitoring to safely initiate hormone therapy. Not everyone is a good candidate for hormone therapy.
Strength Training 2-3 times weekly should be a goal of anyone with an interest in functional longevity. Muscle mass is critical in blood glucose management, mobility and preservation of bone mineral density.
Avoid alcohol, maintain a healthy weight, and don’t smoke. Small daily decisions add up.
Ally: Talk to me about health and social media. TikTok says testosterone fixes everything. Instagram says MHT is dangerous. What should readers do with all the noise?
Dr. Hull: Social media exaggerates and AI hallucinates. Everyone on social media, ESPECIALLY Instagram, is trying to sell you something. Examine the credentials and the profit motives of everyone offering “free” advice. Exaggerated but confident statements drive engagement even if they’re false or misleading. Engagement drives clicks and clicks generate revenue. This is your brain on the Attention Economy.
I always ask my patients who they’re following on social media. The clinic where I see patients offers monthly physician-led teaching sessions and twice-weekly group educational sessions led by our certified Health Coach. We do this, in part, to combat misinformation and provide our patients with reliable, up-to-date knowledge.
My general advice is to fact-check information from the internet with a licensed and preferably certified clinician that you trust. Not ChatGPT; it’s opinions are formed by algorithms which serve the interests of tech company shareholders. I realize that this can be challenging in an over-stressed medical system. If you want to understand my position on AI, I strongly recommend the work of Tristan Harris.
Resources
I have lots of patients who use period tracking apps. I feel confident recommending them here in British Columbia and find the data useful. But I understand the concern about government surveillance of that kind of data in the United States. To date, there are no guardrails on how that data can be accessed and used by law enforcement to prosecute women for their reproductive choices. A reasonable solution for women in the States is to track their periods on a paper calendar. The first day of the period is Day 1 of the cycle in a woman who has regular menses. Her most fertile time (when she’s most likely to become pregnant) is the 5 days before ovulation, the day of ovulation and the day after ovulation. On the calendar below, that would be days 9-15.
In the early stages of the menopause transition, the interval between periods often becomes shorter. Later during the menopause transition, the interval becomes longer. Obviously, the picture is less clear in patients who have a long history of irregular periods or an IUD.
You don’t need a fancy gadget or app to tell you how you’re feeling but there are a bazillion companies that will tell you that you do. There’s a ton of profiteering going on because women are taking their health into their own hands. A lot of this cash-grab culture is directly related to the systemic failure across health systems to recognize and treat the symptoms of menopause.
The Canadian Menopause Society has some wonderful educational videos on their website for free.
The Menopause Society has a searchable practitioner database.
The International Society for the Study of Women’s Sexual Health also has a searchable database.
Thanks to the friends and readers who have reached out lately to check on me. I’ve been a little quiet for a variety of reasons. Like a lot of people, I’ve been reflecting on the enormous changes of 2025. I’ve let go of a lot of things this year that were no longer serving me. Similar to last year, I’ll write a Christmas Love Letter to my paid Subscribers. It will be on the topic of Giving, Receiving and Letting Go.
Wishing you a Blessed Winter Solstice and a Joyful Holiday Season!






